Surgical Technique
The ZIP Flap step-by-step treatment journey
Understanding the ZIP Flap Procedure
The Zygomatic Implant Perforated (ZIP) Flap technique represents a significant advancement in the treatment of upper jaw (maxillary) cancer. It combines tumour removal, reconstruction, and dental rehabilitation into a coordinated treatment pathway—allowing patients to regain function and appearance in weeks rather than years. More importantly, unlike other techniques used for upper jaw cancers , the ZIP Flap using zygomatic implants have proven success when post-operative radiotherapy is used as an adjuvant treatment. Our patient reported quality of life data from this technique has been very encouraging
This page guides you through each stage of the treatment journey, from initial planning through to long-term follow-up. Whether you're a patient exploring treatment options or a medical professional learning about the technique, use the interactive timeline below to explore each stage in detail.
Pre-operative Planning
Assessment, imaging and treatment coordination
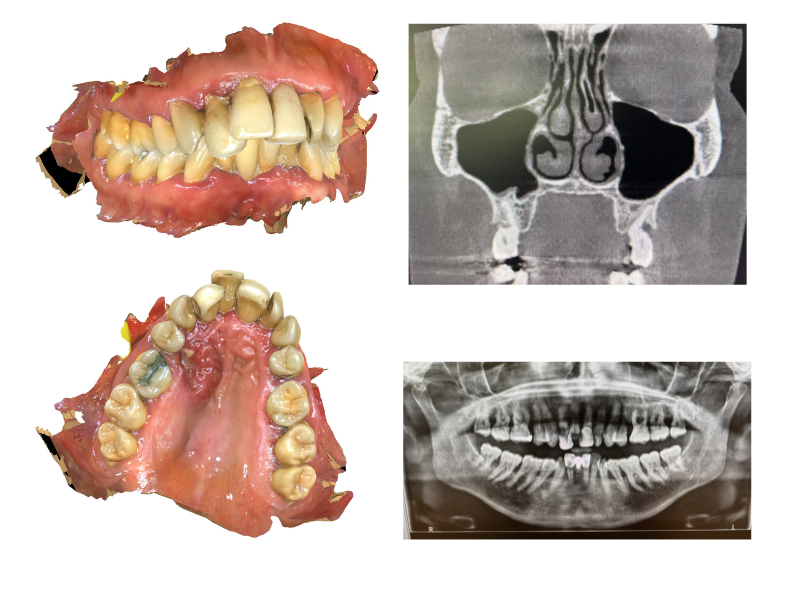
Before surgery, your clinical team will carry out detailed assessments to plan every aspect of your treatment. This includes CT scans and other imaging to map the tumour and surrounding anatomy, along with dental impressions to begin planning your new teeth.
The surgical and prosthodontic teams work together to determine the optimal positions for your implants, ensuring the best possible outcome for both tumour removal and dental restoration.
You'll meet with various members of the multidisciplinary team who will explain the procedure, answer your questions, and help you prepare for surgery and recovery.
Clinical Considerations
High-resolution CT imaging with dental protocol is essential for assessment of zygomatic bone stock and planning implant trajectories. Pre-operative dental impressions and jaw registration allow fabrication of surgical guides and enable prosthodontic planning to commence before surgery.
Two-team operating approach requires coordination between ablative surgeon, reconstructive surgeon, and maxillofacial prosthodontist. Virtual surgical planning may be employed for complex cases.
Assessment should include evaluation of remaining dentition, occlusal scheme, and potential implant sites on the non-defect side for cross-arch stabilisation.
Tumour Resection
Removal of the cancer with safe margins
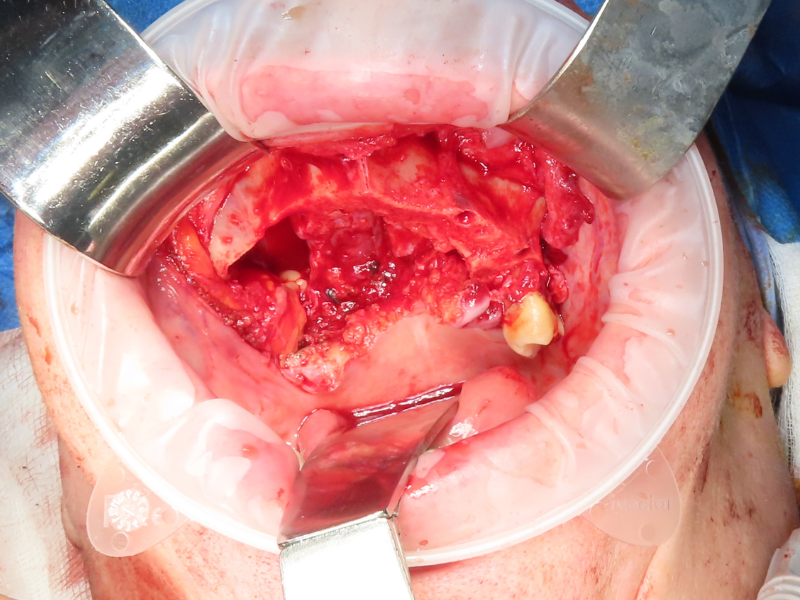
The first priority of surgery is the complete removal of the cancer. The surgeon performs a low-level maxillectomy—removing the affected portion of your upper jaw while carefully preserving key structures such as the eye socket floor and cheekbone (zygoma).
Appropriate oncological margins are taken to ensure all cancerous tissue is removed. If lymph nodes in the neck require treatment, this is addressed during the same operation.
Preserving the zygoma is crucial as this provides the strong bone needed to anchor your new dental implants.
Surgical Approach
Low-level maxillectomy (Brown Class II) with preservation of the orbital floor and zygomatic complex. Resection margins confirmed with frozen section where indicated. Neck dissection performed concurrently if nodal metastasis suspected.
The technique is applicable to tumours requiring infrastructure maxillectomy where zygomatic bone stock is preserved. Careful assessment of posterior and superior margins is essential.
Access typically via Weber-Ferguson incision with lip-split, or transoral approach for smaller defects. Osteotomies planned to maximise residual bone for implant placement.
Zygomatic Implant Placement
Installing the foundations for your new teeth
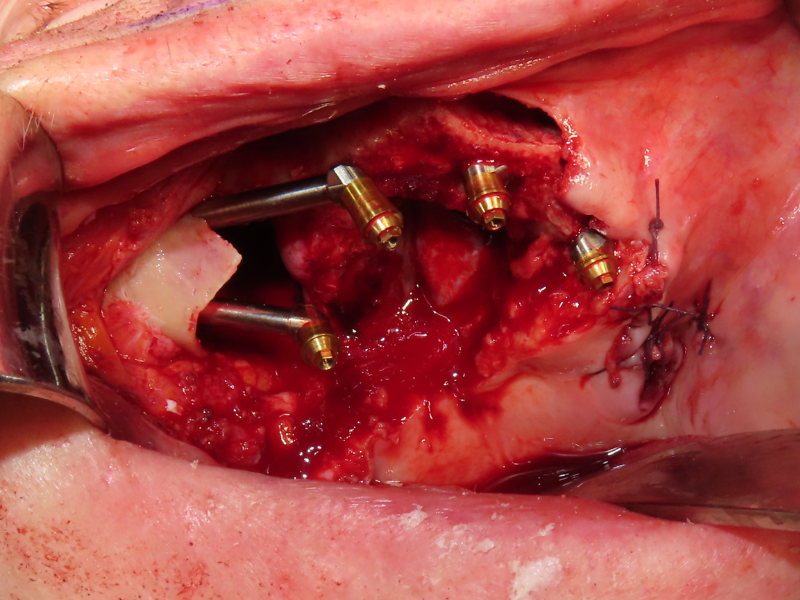
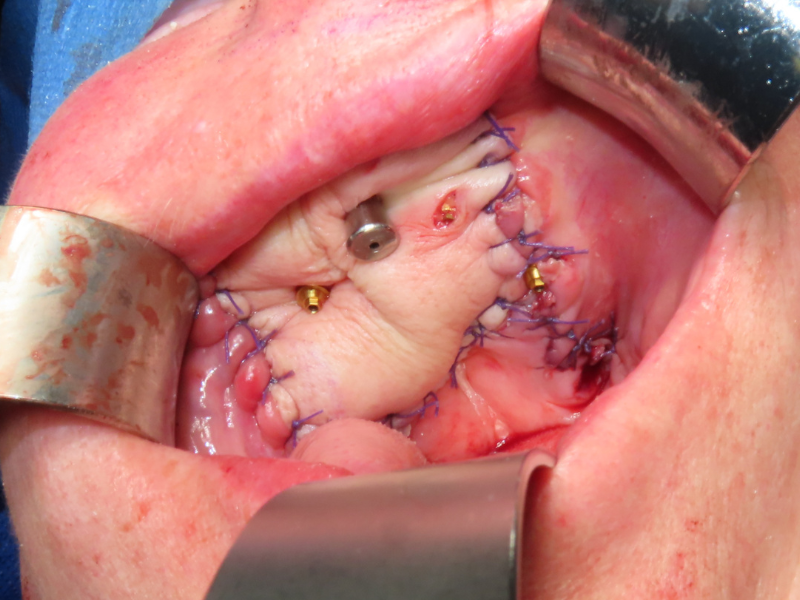
Once the tumour has been removed, specially designed oncology zygomatic implants are placed into your remaining cheekbone (zygoma). These long implants anchor securely into this dense bone, providing a strong foundation for your replacement teeth.
Depending on your specific situation, additional standard dental implants may be placed on the unaffected side of your mouth to provide optimal support for your prosthesis.
The implant placement is done during the same operation as tumour removal, so there's no need for a separate surgery—this is a key advantage of the ZIP Flap approach.
Implant Protocol
Oncology zygomatic implants (typically 2-3 on defect side) placed into residual zygoma with primary stability. Two-team operating allows simultaneous flap harvest while implants are placed. Implant positions planned to allow cross-arch prosthetic fixation.
Additional conventional implants on the non-defect side where bone permits. Removal of teeth adjacent to defect may be required to optimise implant positioning. Multi-unit abutments connected at time of surgery.
Implant trajectory follows zygomatic bone anatomy; extra-sinus approach preferred where possible. Minimum insertion torque of 35Ncm recommended for immediate loading protocol.
Flap Reconstruction
Closing the defect with living tissue
To close the gap left by tumour removal, a microvascular free flap—typically from your forearm (radial forearm free flap) or thigh (ALT flap)—is used. This is living tissue with its own blood supply, which is reconnected to blood vessels in your neck using microsurgical techniques.
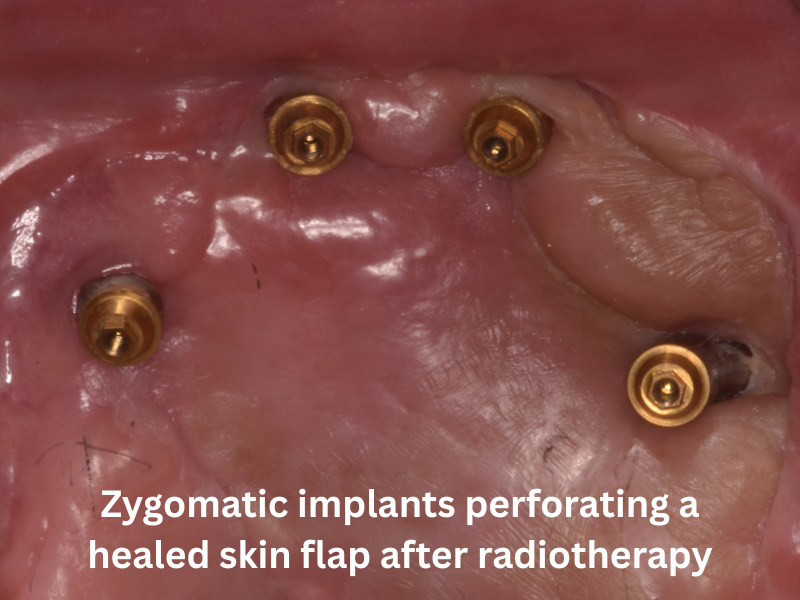
The key innovation of the ZIP Flap technique is that this soft tissue flap is perforated by the implant abutments. Rather than burying the implants under the flap, they pass through it—sealing the surgical defect while keeping the implants accessible for your new teeth.
The donor site (forearm or thigh) is closed directly or with a skin graft, and heals well with minimal long-term impact.
Flap Selection & Technique
Radial forearm free flap (RFFF) or anterolateral thigh (ALT) flap preferred for their pliability and reliable pedicle. Flap raised in parallel by second team during implant placement to reduce operative time.
Flap perforated over abutment positions and secured with protective washer system. Slight oversizing recommended to account for post-radiotherapy shrinkage. Flap inset to achieve oro-nasal separation and provide stable soft tissue around abutments.
Microvascular anastomosis to facial vessels; venous coupler device facilitates rapid anastomosis. Flap monitoring via implantable Doppler or clinical observation.
Prosthesis Fabrication & Loading
Creating and fitting your new teeth
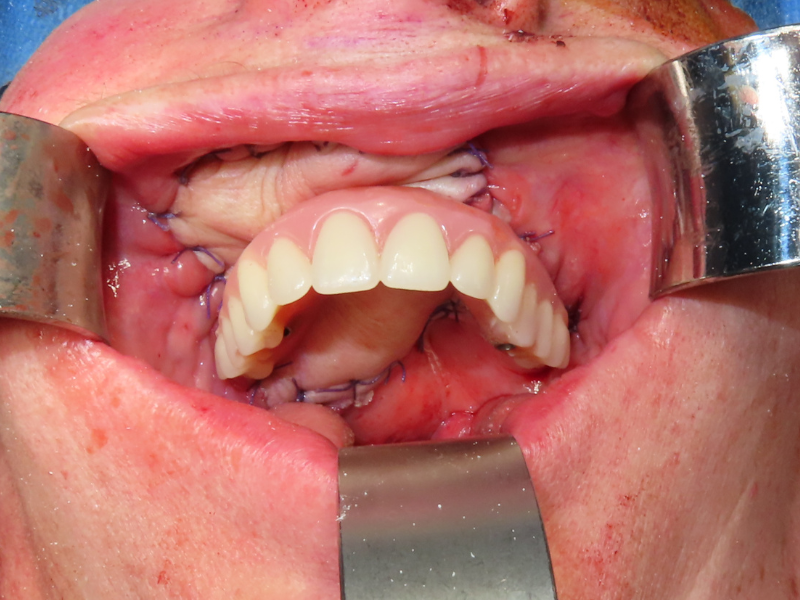
Impressions for your new teeth are taken either during surgery or in the early days of your recovery. This allows the dental laboratory to begin fabricating your fixed prosthesis (bridge) while you're still in the initial healing phase.
Remarkably, your new fixed teeth can typically be fitted within 3-4 weeks of surgery—far faster than traditional approaches which often require many months. This rapid rehabilitation means you can eat, speak, and smile with confidence much sooner.
The prosthesis is securely attached to your implants but can be removed by your dental team for cleaning and maintenance. To you, it looks and functions like natural teeth.
Prosthodontic Protocol
Intra-operative impressions using pick-up copings and closed-tray technique. Jaw registration recorded against remaining dentition or denture. Laboratory fabrication during 2-3 week healing period allows immediate/early loading protocol.
Fixed prosthesis design typically incorporates pink acrylic flange to restore lost alveolar contour. Screw-retained design allows retrievability for hygiene and maintenance. Cross-arch stabilisation essential for managing off-axis loading on zygomatic implants.
Titanium framework with acrylic teeth preferred initially; definitive prosthesis may be fabricated after tissue maturation. Occlusal scheme designed to minimise lateral forces on implants.
Radiotherapy
Additional treatment when required
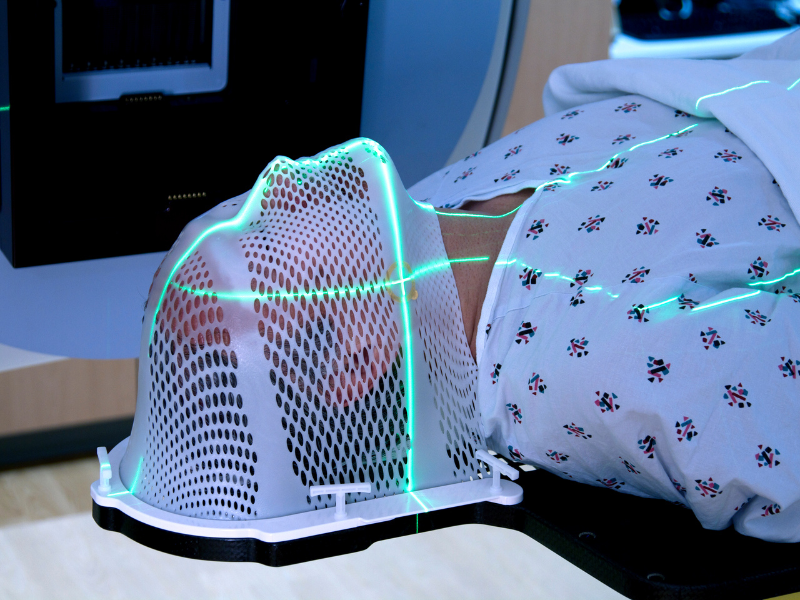
Many patients with maxillary cancer require radiotherapy after surgery to reduce the risk of the cancer returning. A significant advantage of the ZIP Flap technique is that your dental rehabilitation is complete before radiotherapy begins.
This is important because radiotherapy can make future dental implant treatment more difficult and risky. With ZIP Flap, your implants are already placed and integrated, and you have functioning teeth throughout your radiotherapy course.
During radiotherapy, your prosthesis may need minor adjustments as the tissues can change slightly. Your clinical team will support you through this phase and make any modifications needed to keep you comfortable.
Radiotherapy Considerations
Adjuvant radiotherapy typically commences 4-6 weeks post-operatively. Early prosthetic loading allows dental rehabilitation to be complete prior to RT commencement—avoiding the complications of implant placement in irradiated bone.
Flap tissue may exhibit some shrinkage during and after RT; prosthesis may require relining or adjustment. Implant survival in the zygomatic bone (outside the high-dose RT field) has shown excellent results even with post-operative radiotherapy.
IMRT planning should account for implant artefact. Fluoride trays recommended for remaining natural teeth. Salivary dysfunction management may be required.
Long-term Follow-up
Ongoing care and monitoring
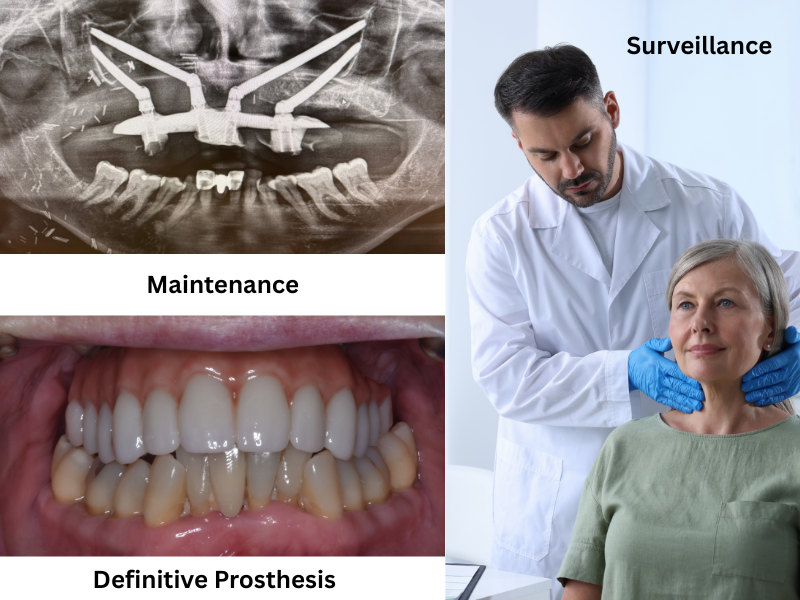
After completing your initial treatment, you'll have regular follow-up appointments with both your cancer team and your dental team. These visits monitor for any signs of cancer recurrence and ensure your implants and prosthesis continue to function well.
Your prosthesis will need periodic professional cleaning and maintenance—typically every 3-6 months. The dental team will remove it, clean around the implants, and check everything is healthy before refitting it.
With proper care, your implant-supported prosthesis can last many years, giving you confidence in your appearance and the ability to eat and speak normally. Most patients report significant improvements in their quality of life compared to traditional obturator prostheses.
Maintenance Protocol
Regular oncological surveillance per institutional protocol—typically 3-monthly in year 1, reducing frequency over subsequent years. Prosthodontic review every 3-6 months for professional cleaning and assessment of peri-implant tissues.
Published outcomes demonstrate 100% flap survival, 98.4% implant survival, and significant improvements in patient-reported outcome measures (UWQOL, LORQ) compared to baseline and traditional obturator rehabilitation.
Mean time to prosthesis delivery approximately 29 days. Long-term data shows sustained functional outcomes and patient satisfaction at 5+ years follow-up.
ZIP Flap Timeline
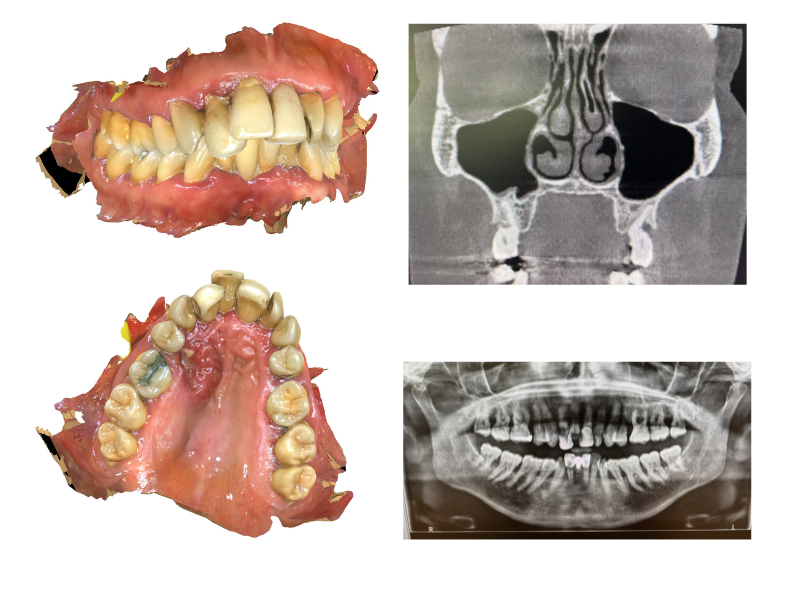
Before surgery, your clinical team will carry out detailed assessments to plan every aspect of your treatment. This includes CT scans and other imaging to map the tumour and surrounding anatomy, along with dental impressions to begin planning your new teeth.
The surgical and prosthodontic teams work together to determine the optimal positions for your implants, ensuring the best possible outcome for both tumour removal and dental restoration.
You'll meet with various members of the multidisciplinary team who will explain the procedure, answer your questions, and help you prepare for surgery and recovery.
Clinical Considerations
High-resolution CT imaging with dental protocol is essential for assessment of zygomatic bone stock and planning implant trajectories. Pre-operative dental impressions and jaw registration allow fabrication of surgical guides and enable prosthodontic planning to commence before surgery.
Two-team operating approach requires coordination between ablative surgeon, reconstructive surgeon, and maxillofacial prosthodontist. Virtual surgical planning may be employed for complex cases.
Assessment should include evaluation of remaining dentition, occlusal scheme, and potential implant sites on the non-defect side for cross-arch stabilisation.
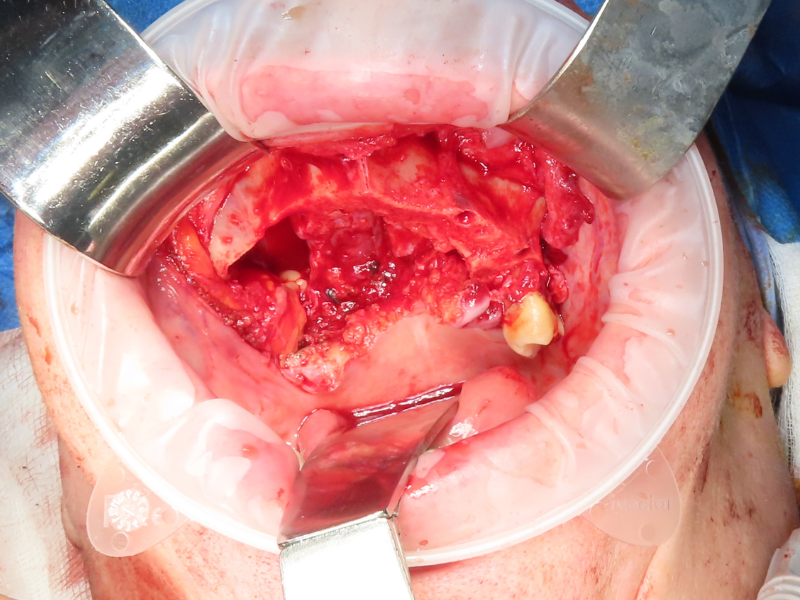
The first priority of surgery is the complete removal of the cancer. The surgeon performs a low-level maxillectomy—removing the affected portion of your upper jaw while carefully preserving key structures such as the eye socket floor and cheekbone (zygoma).
Appropriate oncological margins are taken to ensure all cancerous tissue is removed. If lymph nodes in the neck require treatment, this is addressed during the same operation.
Preserving the zygoma is crucial as this provides the strong bone needed to anchor your new dental implants.
Surgical Approach
Low-level maxillectomy (Brown Class II) with preservation of the orbital floor and zygomatic complex. Resection margins confirmed with frozen section where indicated. Neck dissection performed concurrently if nodal metastasis suspected.
The technique is applicable to tumours requiring infrastructure maxillectomy where zygomatic bone stock is preserved. Careful assessment of posterior and superior margins is essential.
Access typically via Weber-Ferguson incision with lip-split, or transoral approach for smaller defects. Osteotomies planned to maximise residual bone for implant placement.
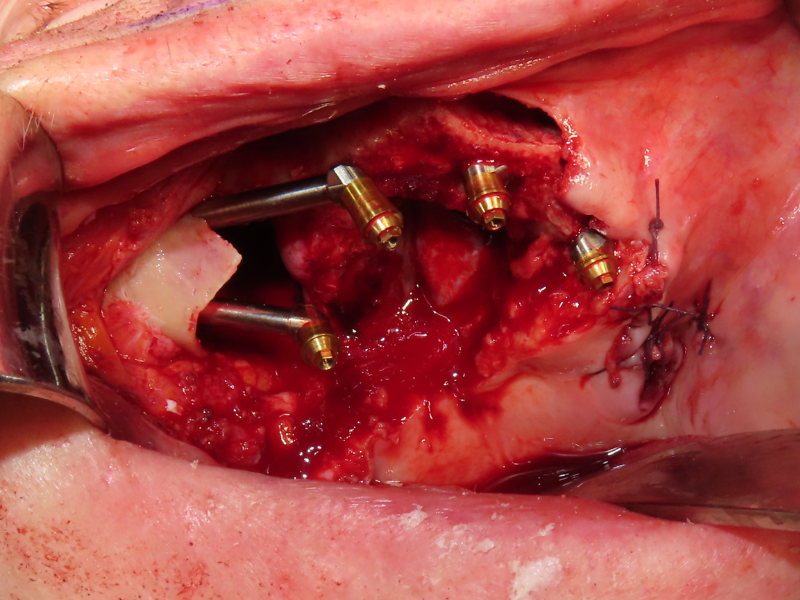
Once the tumour has been removed, specially designed oncology zygomatic implants are placed into your remaining cheekbone (zygoma). These long implants anchor securely into this dense bone, providing a strong foundation for your replacement teeth.
Depending on your specific situation, additional standard dental implants may be placed on the unaffected side of your mouth to provide optimal support for your prosthesis.
The implant placement is done during the same operation as tumour removal, so there's no need for a separate surgery—this is a key advantage of the ZIP Flap approach.
Implant Protocol
Oncology zygomatic implants (typically 2-3 on defect side) placed into residual zygoma with primary stability. Two-team operating allows simultaneous flap harvest while implants are placed. Implant positions planned to allow cross-arch prosthetic fixation.
Additional conventional implants on the non-defect side where bone permits. Removal of teeth adjacent to defect may be required to optimise implant positioning. Multi-unit abutments connected at time of surgery.
Implant trajectory follows zygomatic bone anatomy; extra-sinus approach preferred where possible. Minimum insertion torque of 35Ncm recommended for immediate loading protocol.
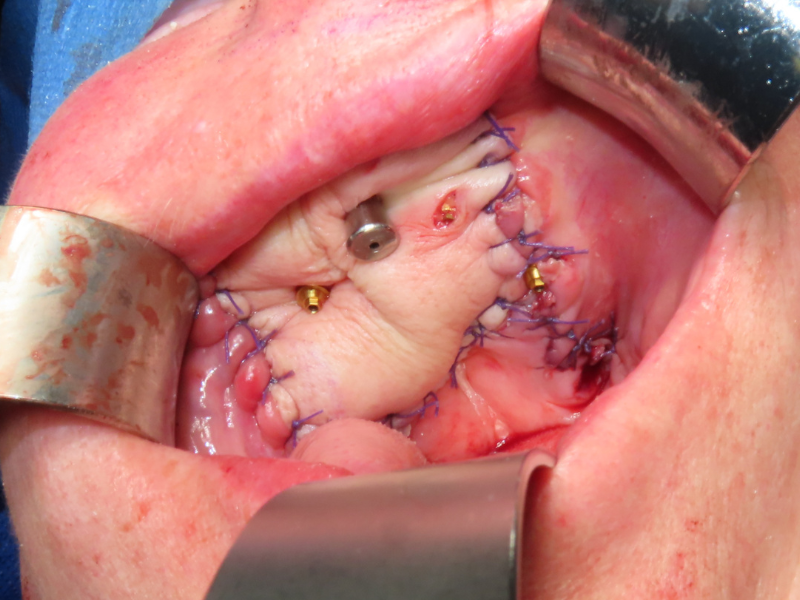
To close the gap left by tumour removal, a microvascular free flap—typically from your forearm (radial forearm free flap) or thigh (ALT flap)—is used. This is living tissue with its own blood supply, which is reconnected to blood vessels in your neck using microsurgical techniques.
The key innovation of the ZIP Flap technique is that this soft tissue flap is perforated by the implant abutments. Rather than burying the implants under the flap, they pass through it—sealing the surgical defect while keeping the implants accessible for your new teeth.
The donor site (forearm or thigh) is closed directly or with a skin graft, and heals well with minimal long-term impact.
Flap Selection & Technique
Radial forearm free flap (RFFF) or anterolateral thigh (ALT) flap preferred for their pliability and reliable pedicle. Flap raised in parallel by second team during implant placement to reduce operative time.
Flap perforated over abutment positions and secured with protective washer system. Slight oversizing recommended to account for post-radiotherapy shrinkage. Flap inset to achieve oro-nasal separation and provide stable soft tissue around abutments.
Microvascular anastomosis to facial vessels; venous coupler device facilitates rapid anastomosis. Flap monitoring via implantable Doppler or clinical observation.
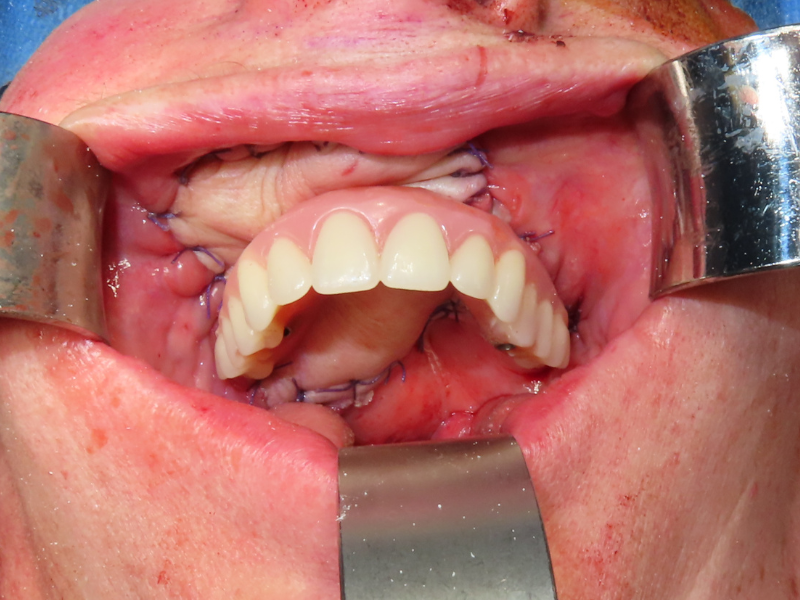
Impressions for your new teeth are taken either during surgery or in the early days of your recovery. This allows the dental laboratory to begin fabricating your fixed prosthesis (bridge) while you're still in the initial healing phase.
Remarkably, your new fixed teeth can typically be fitted within 3-4 weeks of surgery—far faster than traditional approaches which often require many months. This rapid rehabilitation means you can eat, speak, and smile with confidence much sooner.
The prosthesis is securely attached to your implants but can be removed by your dental team for cleaning and maintenance. To you, it looks and functions like natural teeth.
Prosthodontic Protocol
Intra-operative impressions using pick-up copings and closed-tray technique. Jaw registration recorded against remaining dentition or denture. Laboratory fabrication during 2-3 week healing period allows immediate/early loading protocol.
Fixed prosthesis design typically incorporates pink acrylic flange to restore lost alveolar contour. Screw-retained design allows retrievability for hygiene and maintenance. Cross-arch stabilisation essential for managing off-axis loading on zygomatic implants.
Titanium framework with acrylic teeth preferred initially; definitive prosthesis may be fabricated after tissue maturation. Occlusal scheme designed to minimise lateral forces on implants.
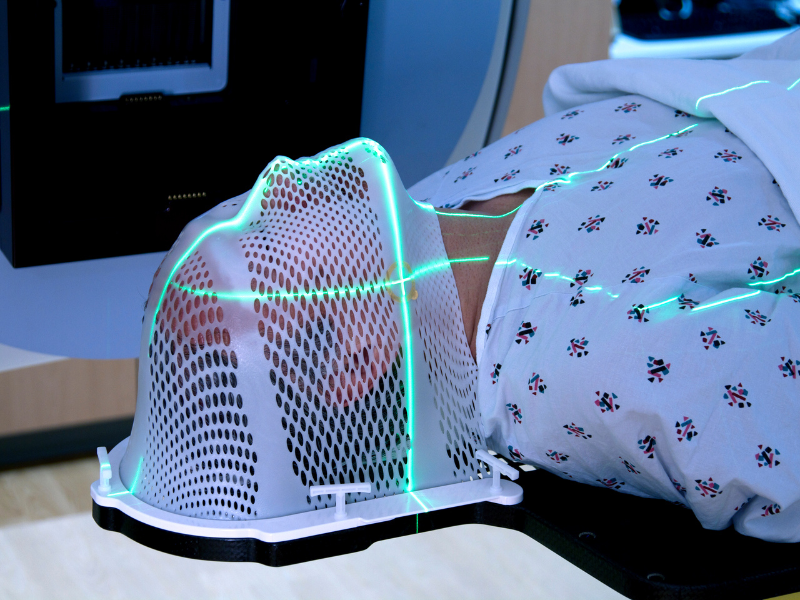
Many patients with maxillary cancer require radiotherapy after surgery to reduce the risk of the cancer returning. A significant advantage of the ZIP Flap technique is that your dental rehabilitation is complete before radiotherapy begins.
This is important because radiotherapy can make future dental implant treatment more difficult and risky. With ZIP Flap, your implants are already placed and integrated, and you have functioning teeth throughout your radiotherapy course.
During radiotherapy, your prosthesis may need minor adjustments as the tissues can change slightly. Your clinical team will support you through this phase and make any modifications needed to keep you comfortable.
Radiotherapy Considerations
Adjuvant radiotherapy typically commences 4-6 weeks post-operatively. Early prosthetic loading allows dental rehabilitation to be complete prior to RT commencement—avoiding the complications of implant placement in irradiated bone.
Flap tissue may exhibit some shrinkage during and after RT; prosthesis may require relining or adjustment. Implant survival in the zygomatic bone (outside the high-dose RT field) has shown excellent results even with post-operative radiotherapy.
IMRT planning should account for implant artefact. Fluoride trays recommended for remaining natural teeth. Salivary dysfunction management may be required.
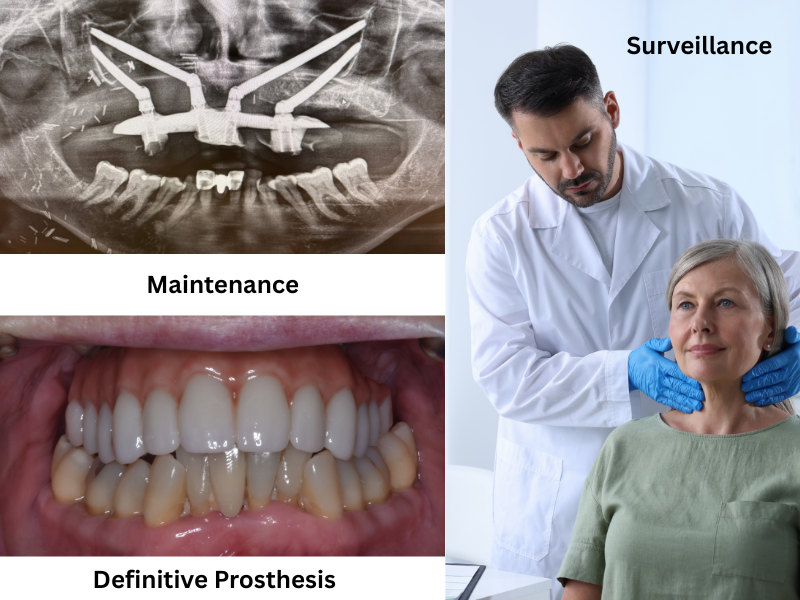
After completing your initial treatment, you'll have regular follow-up appointments with both your cancer team and your dental team. These visits monitor for any signs of cancer recurrence and ensure your implants and prosthesis continue to function well.
Your prosthesis will need periodic professional cleaning and maintenance—typically every 3-6 months. The dental team will remove it, clean around the implants, and check everything is healthy before refitting it.
With proper care, your implant-supported prosthesis can last many years, giving you confidence in your appearance and the ability to eat and speak normally. Most patients report significant improvements in their quality of life compared to traditional obturator prostheses.
Maintenance Protocol
Regular oncological surveillance per institutional protocol—typically 3-monthly in year 1, reducing frequency over subsequent years. Prosthodontic review every 3-6 months for professional cleaning and assessment of peri-implant tissues.
Published outcomes demonstrate 100% flap survival, 98.4% implant survival, and significant improvements in patient-reported outcome measures (UWQOL, LORQ) compared to baseline and traditional obturator rehabilitation.
Mean time to prosthesis delivery approximately 29 days. Long-term data shows sustained functional outcomes and patient satisfaction at 5+ years follow-up.
Learn More About the ZIP Flap Technique
For detailed research and clinical outcomes, explore our publications and case reports. Healthcare professionals interested in training can find course information below.